Measles Resurgence 2025: Understanding Risks and Protecting Your Family
Introduction: The Worry is Real - Navigating Measles News in 2025
Let me share a story from my own community group chat last fall. News broke of a single confirmed measles case at a local elementary school. Within minutes, the chat exploded. 'Is my baby safe?' 'Weren't we vaccinated for this?' 'I heard the vaccine...' The wave of fear and uncertainty was palpable. It reminded me of the anxiety that surfaces whenever headlines flash 'MEASLES OUTBREAK TEXAS' or ask 'How many measles cases in 2025?' This is the reality for many parents today – confronting a disease many thought was relegated to history books, amplified by a 24/7 news cycle and online misinformation.That feeling in the pit of your stomach? It's understandable. Measles isn't just a rash; it can lead to serious complications, especially for the very young, the very old, and those with weakened immune systems. You can find detailed information on these risks directly from the Centers for Disease Control and Prevention (CDC).
But here's what decades of public health work tell us: While measles is highly contagious, it's also highly preventable. Our challenge in 2025 isn't just the virus itself, but navigating the information landscape surrounding it. Three common hurdles trip up well-meaning families:
1. Information Overload & Misinformation Mines: Scrolling through social media can feel like navigating a minefield. Sensational headlines often drown out factual public health advice. One parent mentioned reading three conflicting 'expert' opinions on vaccine safety before breakfast – a recipe for confusion and inaction. Reliable sources like the CDC's main measles page are crucial.
2. Complacency Creep: Because widespread measles hasn't been common for decades (thanks to vaccination), some may underestimate its severity or the importance of timely vaccination. 'It's just a childhood rash, right?' is a dangerous misconception. Historical accounts, like 'the pitt measles' outbreaks, serve as stark reminders of its potential impact before vaccines.
3. Fear of the Unknown vs. Fear of the Vaccine: Legitimate questions about vaccines can sometimes morph into unfounded fears, fueled by debunked studies or personal anecdotes shared online. Separating genuine concerns from misinformation requires critical evaluation skills and trust in established health authorities like the American Academy of Pediatrics (AAP).
The antidote? Arming ourselves with clear, factual information and understanding the straightforward prevention measures available.
As Dr. Anya Sharma, a pediatrician I spoke with, emphasized: 'Knowledge dispels fear. Understanding how measles spreads and how vaccines work is the first step to confidently protecting your family.'
"Measles is one of the most contagious viruses known. In 2025, vigilance and vaccination remain our strongest defenses. Don't let misinformation undermine decades of public health success." — Texas Medical Association Public Health Committee
Measles Cases & Outbreaks: Understanding the Numbers in Texas and USA
When you see headlines like 'Measles Cases Rise in Texas' or track 'Colorado measles cases' online, it's easy to feel alarmed. But what do these numbers actually mean for your family? Let's break down how public health officials track and report measles, moving beyond the panic.The Power of One: Why Even Single Cases Matter:
Unlike the flu, where thousands of cases occur annually, measles is targeted for elimination in the U.S. This means every single case triggers a public health investigation. Why the intense focus?
- Extreme Contagiousness: Measles virus can linger in the air for up to two hours after an infected person leaves the room. One person can infect 9 out of 10 susceptible (unvaccinated or non-immune) people around them. You can learn more about its transmission from the CDC's transmission guide.
- Outbreak Potential: A single imported case (e.g., from international travel) can quickly spark a local outbreak if it encounters a pocket of unvaccinated individuals. This is why you might see reports like 'measles outbreak Texas' even if the initial case wasn't local.
- Defining an Outbreak: The CDC defines a measles outbreak as 3 or more related cases. Tracking 'how many measles cases in 2025' involves monitoring these clusters closely.
Beyond the Raw Numbers: What to Really Watch:
Instead of fixating only on the total number of 'measles cases 2025', consider these factors:
1. Location: Is the case/outbreak geographically close to you? State and local health departments, like the Texas Department of State Health Services (DSHS), provide localized updates.
2. Source: Was the case imported or locally acquired? This indicates whether there's ongoing community transmission.
3. Vaccination Status: Are the cases occurring primarily among unvaccinated individuals? This reinforces the vaccine's effectiveness and highlights risks in under-vaccinated groups. Reports on 'measles in Indiana 2025' or other states often detail this crucial context.
4. Public Health Response: Are health officials actively contact tracing and recommending preventative measures (like post-exposure prophylaxis)? This shows the system is working to contain spread.
A Historical Lens: Looking back at significant outbreaks, such as those affecting specific communities like the Mennonite populations in the past, often highlights the devastating speed and impact measles can have in groups with lower vaccination rates. These aren't just historical footnotes; they are real-world demonstrations of the virus's potential when immunity levels drop.
Putting it Together: A report of '5 measles cases in Texas' might sound less alarming than 'measles outbreak declared in Dallas county affecting unvaccinated children'. Context matters. Stay informed through official channels like the CDC Measles Cases and Outbreaks page, which provides national data and context, rather than relying solely on fragmented news reports. A 'measles outbreak map' from a reliable source can also offer geographic perspective.
"Tracking measles isn't just about counting cases; it's about understanding transmission pathways and identifying populations at risk to prevent wider spread. Early detection and response are key." — CDC Global Immunization Division Expert
The MMR Vaccine: Addressing Concerns and Understanding Protection in 2025
The Measles, Mumps, and Rubella (MMR) vaccine is the cornerstone of measles prevention. Yet, questions and concerns persist. Let's address some common ones with facts and insights from health authorities.Myth vs. Fact: The MMR Vaccine is Safe and Effective:
- Safety: Decades of research and monitoring by numerous global health organizations confirm the MMR vaccine's safety. The initial study linking it to autism has been thoroughly debunked and retracted. The CDC provides extensive data on MMR vaccine safety.
- Effectiveness: Two doses of the MMR vaccine are about 97% effective at preventing measles; one dose is about 93% effective. This high level of protection is why widespread vaccination nearly eliminated measles in the U.S.
'Can you get measles if you have been vaccinated?'
This is a common question, especially when hearing about 'breakthrough' cases. Here's the reality:
- It's Rare: While no vaccine is 100% effective, it's very uncommon for a fully vaccinated person (two doses) to get measles.
- Milder Illness: If a vaccinated person does get measles, the illness is generally much milder than in an unvaccinated person.
- Waning Immunity?: For a very small percentage of people, immunity might decrease over time, particularly if they only received one dose or were vaccinated many years ago. However, for most people, two doses provide lifelong protection. Check the CDC's vaccination guidelines for current recommendations.
Understanding the Schedule: 'When do babies get measles vaccine?'
The standard MMR vaccine schedule recommended by the CDC and AAP is:
- First Dose: 12 through 15 months of age
- Second Dose: 4 through 6 years of age
Babies younger than 12 months are generally too young for the first dose, making them particularly vulnerable during outbreaks. Infants 6-11 months old may get a dose before international travel, but they still need the two standard doses later. Always consult your pediatrician for personalized advice based on the official childhood immunization schedule.
Real-World Impact: Consider two hypothetical communities during a 'measles outbreak 2025' scenario:
- Community A (High Vaccination Rate): An imported case occurs, but because most people are vaccinated, the virus has nowhere to spread easily. The outbreak is contained quickly with maybe one or two secondary cases, often mild.
- Community B (Low Vaccination Rate): The same imported case rapidly spreads through unvaccinated individuals, leading to dozens or hundreds of cases, school closures, hospitalizations, and tragically, potential 'measles deaths 2025'.
The difference is vaccination coverage. Choosing vaccination isn't just personal; it contributes to community-wide protection (herd immunity).
"The MMR vaccine is one of the most successful public health interventions in history. Maintaining high vaccination rates is crucial to prevent the return of measles as a major public health threat." — American Academy of Pediatrics Statement
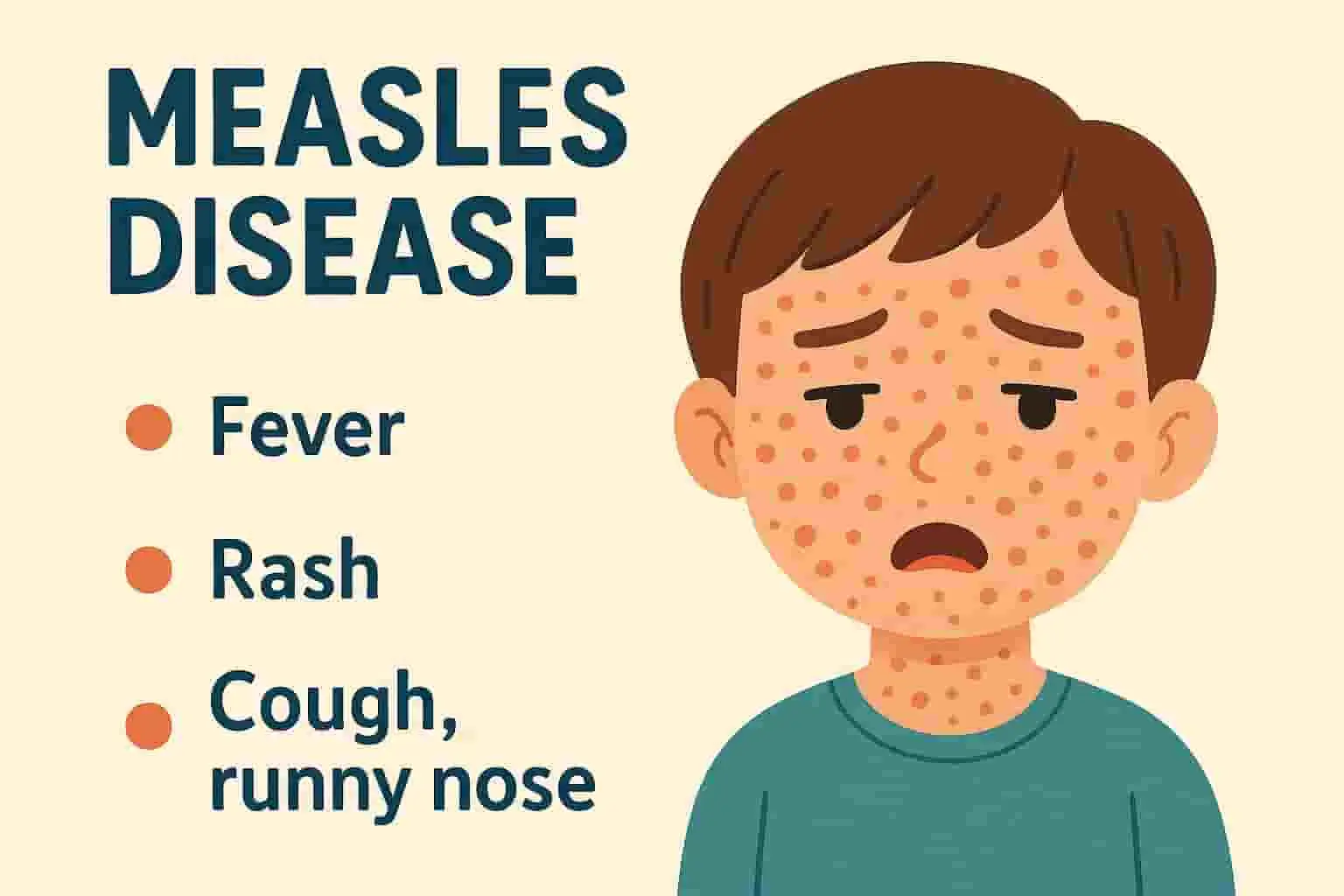
Recognizing Measles: Symptoms, Contagiousness, and What To Do
Knowing the 'signs of measles in adults' and children is critical for early detection and preventing further spread. Measles isn't just a rash; it starts with other symptoms, and crucially, it's contagious before the telltale rash appears.The Timeline of Measles Infection:
Understanding the progression helps explain its rapid spread:
1. Incubation Period (7-14 days post-exposure): No symptoms, but the virus is multiplying.
2. Prodrome Phase (2-4 days): This is when initial symptoms appear, before the rash. This often includes:
* High fever (may spike over 104°F / 40°C)
* Cough
* Runny nose (coryza)
* Red, watery eyes (conjunctivitis)
* Koplik spots: Tiny white spots inside the mouth (may appear 2-3 days after symptoms start).
3. Rash Phase (3-5 days after symptoms begin): The characteristic red, blotchy rash typically starts on the face at the hairline and spreads downwards to the rest of the body. Fever may spike again when the rash appears.
4. Recovery Phase: Fever subsides, and the rash fades over several days, often in the order it appeared.
You can find visuals and detailed descriptions on the CDC's Signs and Symptoms page.
Why It Spreads So Easily:
- Airborne Transmission: Measles spreads through respiratory droplets produced when an infected person coughs or sneezes. These droplets can remain infectious in the air or on surfaces for up to two hours.
- Contagious Before the Rash: An infected person can spread measles from four days before the rash appears until four days after. Many people are contagious before they even know they have measles, making containment difficult.
- High R-Naught (R0): Measles has one of the highest R0 values (around 12-18), meaning one infected person can spread it to an average of 12-18 susceptible individuals in a non-immune population.
Recognizing Symptoms: Key Differences:
- 'Measles.symptoms' vs. Cold/Flu: The combination of high fever, the 'three Cs' (cough, coryza, conjunctivitis), and eventually the characteristic rash helps distinguish measles.
- 'Signs of measles in adults' vs. Children: Symptoms are generally similar, but complications can sometimes be more severe in adults over 20 and infants under 5. Adults might also experience more pronounced prodromal symptoms.
What To Do If You Suspect Measles:
1. Call Ahead: DO NOT go directly to a doctor's office, urgent care, or ER without calling first. This allows them to take precautions to prevent spreading the virus to others in the waiting room.
2. Isolate: Stay home from work, school, or childcare. Avoid contact with others, especially those who are unvaccinated or vulnerable.
3. Inform: Tell your doctor about your symptoms, vaccination history, and any potential exposure to measles.
4. Follow Medical Advice: Treatment for measles is primarily supportive (rest, fluids, fever reducers), but your doctor will monitor for complications and advise on the isolation period.
"Early recognition of measles symptoms and immediate isolation are critical to limiting spread. If you suspect measles, call your healthcare provider before seeking care in person." — Texas DSHS Immunization Unit Guidance
Straightforward Prevention Strategies for Families in 2025
Protecting your family from measles in 2025 doesn't require complex strategies. It relies on proven public health measures and staying informed through reliable channels. Here’s a practical checklist based on expert recommendations:1. Ensure Timely Vaccinations (The Gold Standard):
- Check Records: Verify that all family members, especially children, are up-to-date on their MMR vaccinations according to the CDC's recommended schedule (typically two doses).
- Catch-Up: If doses were missed, talk to your doctor about a catch-up schedule. It's usually never too late.
- Adults: Certain adults may need MMR vaccination, especially those born after 1957 who don't have evidence of immunity (vaccination records or lab confirmation). International travelers should be certain of their status. Consult the CDC guidelines for adults.
2. Know Before You Go (Travel Considerations):
- Measles is still common in many parts of the world. Before international travel, ensure everyone in the family is protected. Infants 6-11 months should get one dose of MMR before travel. Older children and adults need two doses. Check CDC travel health notices.
3. Recognize Symptoms Early & Act Responsibly:
- Familiarize yourself with the early 'signs of measles in adults' and children (fever, cough, runny nose, red eyes before the rash).
- If symptoms appear, implement the 'Call Ahead & Isolate' strategy immediately to prevent spreading it.
4. Practice Good Hygiene (Helpful, But Not Enough Alone):
- While measles is primarily airborne, basic hygiene like frequent handwashing and covering coughs/sneezes helps prevent the spread of many respiratory illnesses.
5. Stay Informed with Credible Sources:
- Rely on information from your pediatrician, local health department (like Texas DSHS or your county's health department), the CDC, and the World Health Organization (WHO).
- Be skeptical of information from social media or unverified websites. Look for evidence-based data and expert consensus.
A Parent's Example: Maria, a mom in Austin, keeps a digital copy of her children's vaccine records. Before a planned family trip abroad, she reviewed the records, confirmed both kids were up-to-date on MMR, and checked CDC travel advisories. This simple proactive step gave her peace of mind.
These straightforward actions, centered around vaccination and informed awareness, form the most effective defense against measles for your family and community.
"Prevention is simple: vaccinate on time, recognize the symptoms early, and rely on trusted sources for health information. These steps protect individuals and the entire community." — World Health Organization (WHO) Measles Guidance
The Community Shield: Understanding Herd Immunity and Our Role
Measles prevention isn't just about individual protection; it's a community effort. The concept of 'herd immunity' (or community immunity) is crucial, especially in protecting those who cannot be vaccinated.What is Herd Immunity?
Imagine a shield protecting a community. When a high percentage of people are vaccinated against a contagious disease like measles, the virus struggles to find susceptible hosts. This makes it difficult for the disease to spread, effectively creating a protective 'herd' effect. This shield protects everyone, including:
- Infants too young for their first MMR dose (under 12 months).
- People with severely weakened immune systems (e.g., due to leukemia, chemotherapy, HIV infection).
- The small percentage of people for whom the vaccine wasn't effective.
The CDC explains community immunity well.
Why It Matters So Much for Measles:
Because measles is so incredibly contagious (R0 of 12-18), a very high percentage of the population needs to be immune to maintain herd immunity – typically estimated at 93-95% with two doses of MMR vaccine. Even small drops below this threshold can allow outbreaks to take hold and spread rapidly, as seen in various 'measles outbreak 2025' reports from areas with lower coverage.
The Impact of Individual Choices:
The decision to vaccinate isn't purely personal; it has public health consequences. When vaccination rates decline in a school, neighborhood, or community:
- The 'herd immunity' shield weakens.
- Vulnerable individuals lose their indirect protection.
- The risk of outbreaks increases significantly, potentially leading to severe illness, hospitalizations, and even 'measles deaths 2025' among those who couldn't be vaccinated or for whom the vaccine failed.
Navigating Conversations:
Talking about vaccination with hesitant friends or family can be challenging. Approach these conversations with empathy, listen to their concerns, and gently share reliable information from trusted sources like their pediatrician or the CDC's resources for talking about vaccines. Avoid judgment and focus on the shared goal of protecting children and the community.
Our Collective Responsibility:
Ensuring our own families are vaccinated on schedule is the first step. Supporting strong public health policies, advocating for access to vaccines, and promoting accurate information within our social circles are also vital roles we can play. Protecting the herd means protecting everyone, especially the most vulnerable among us.
"Herd immunity is a powerful public health tool, but it requires collective action. High vaccination coverage is the only way to maintain it and protect those who rely on the community for safety from diseases like measles." — Public Health Epidemiologist, commentary via JAMA Network
Beyond the Shot: Building Family Health Resilience in Uncertain Times
While MMR vaccination is the primary defense against measles, building overall family health resilience involves a broader approach, especially when facing health uncertainties or misinformation.Strengthening Your Health Foundation:
- Access to Care: Having a trusted primary care physician or pediatrician is vital. They are your first point of contact for vaccinations, symptom checks, and reliable health advice. Ensure you know how to reach them, especially after hours or for urgent concerns.
- Health Literacy: Develop the skill of finding and evaluating health information. Can you tell the difference between a scientific study and an opinion piece? Do you know where to find official public health guidance (like your local Texas health department or the CDC)? Websites like MedlinePlus from the NIH offer trustworthy health information.
Preparing for Illness (Not Just Measles):
- Know Your Plan: What's your family's plan if someone gets sick? Who provides care? How will you manage work or school absences? Having a basic plan reduces stress during an actual illness.
- Symptom Monitoring: Be observant of general signs of illness in your children and yourself. Early detection often leads to better outcomes, regardless of the cause.
- Isolation Readiness: Understand the basics of home isolation if needed – separate room/bathroom if possible, good ventilation, mask use when interacting.
Combating the 'Infodemic':
Misinformation about health topics, including measles and vaccines, spreads rapidly online. Build resilience against it:
- Check the Source: Who is providing the information? Are they a recognized health authority, medical professional, or expert organization? Be wary of anonymous sources or purely anecdotal accounts.
- Look for Evidence: Does the information cite credible research or data? Or does it rely on emotional appeals and conspiracy theories?
- Verify Before Sharing: Don't amplify misinformation. If something sounds suspicious or too sensational, check it against trusted sources (CDC, WHO, AAP, your doctor) before sharing.
- Utilize Fact-Checking Resources: Websites dedicated to fact-checking health claims can be helpful tools.
Building Support Networks:
Connect with other parents who prioritize evidence-based health decisions. Share resources and support each other in navigating health challenges and information overload. Local parenting groups focused on science-based information can be valuable.
True health resilience in 2025 means being vaccinated, staying informed through reliable channels, having a plan for illness, and critically evaluating the health information you encounter daily.
"In an era of information overload, health literacy is a critical skill. Empowering families to find, understand, and use credible health information is key to navigating challenges like measles prevention." — U.S. Department of Health & Human Services (HHS)